8 things to know about direct-to-consumer health tests
“Demand better for your body,” says Everlywell, which offers “easy, affordable, & private lab testing without leaving home.”
“You’re already doing so much to track your health,” says gene-testing giant 23andMe. “Add personalized DNA insights for a more complete picture of your health.”
Are direct-to-consumer health tests worth it?
Step right up. Learn about your health from the comfort of your home without ever seeing a doctor. Just send in a urine, saliva, or blood sample, and you’re on the path to knowing more about you.
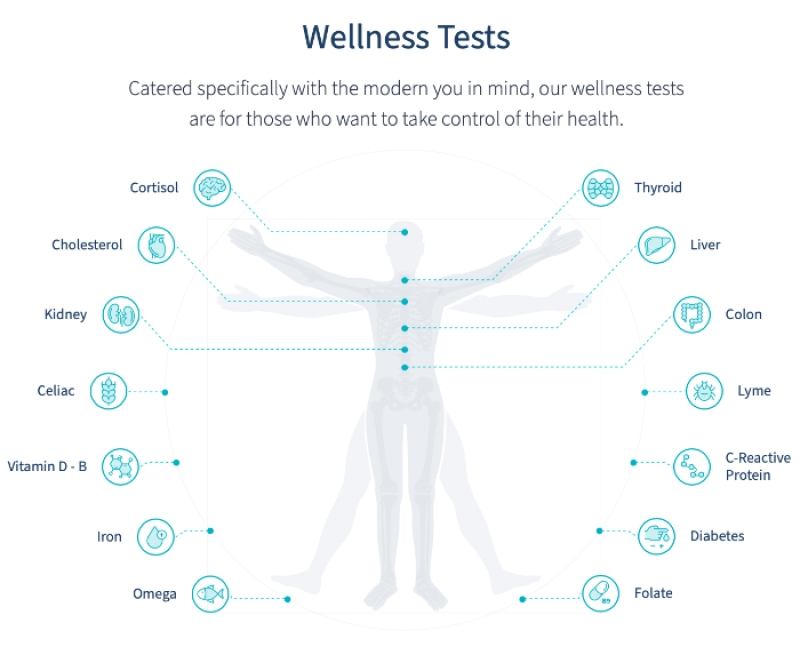
Do you have Lyme disease or HIV? How’s your vitamin D? Your cholesterol? Your estrogen levels? Do your genes make you more likely to get late-onset Alzheimer’s?
“In theory, I like the idea of direct-to-consumer testing,” says Rashmi Mullur, an endocrinologist and assistant professor of medicine at UCLA. “The thought of not having to go into a lab to get a blood test is so appealing.”
“But I worry that some patients are taking these tests out of frustration because they haven’t found an answer through traditional systems, and they feel compelled to take matters into their own hands.”
What’s more, adds Mullur, “some of these tests are not ready for prime time.”
Here’s what to know before you spit into that sample vial.
1. Beware the limitations
The stakes for some tests are far too high to risk a wrong answer.
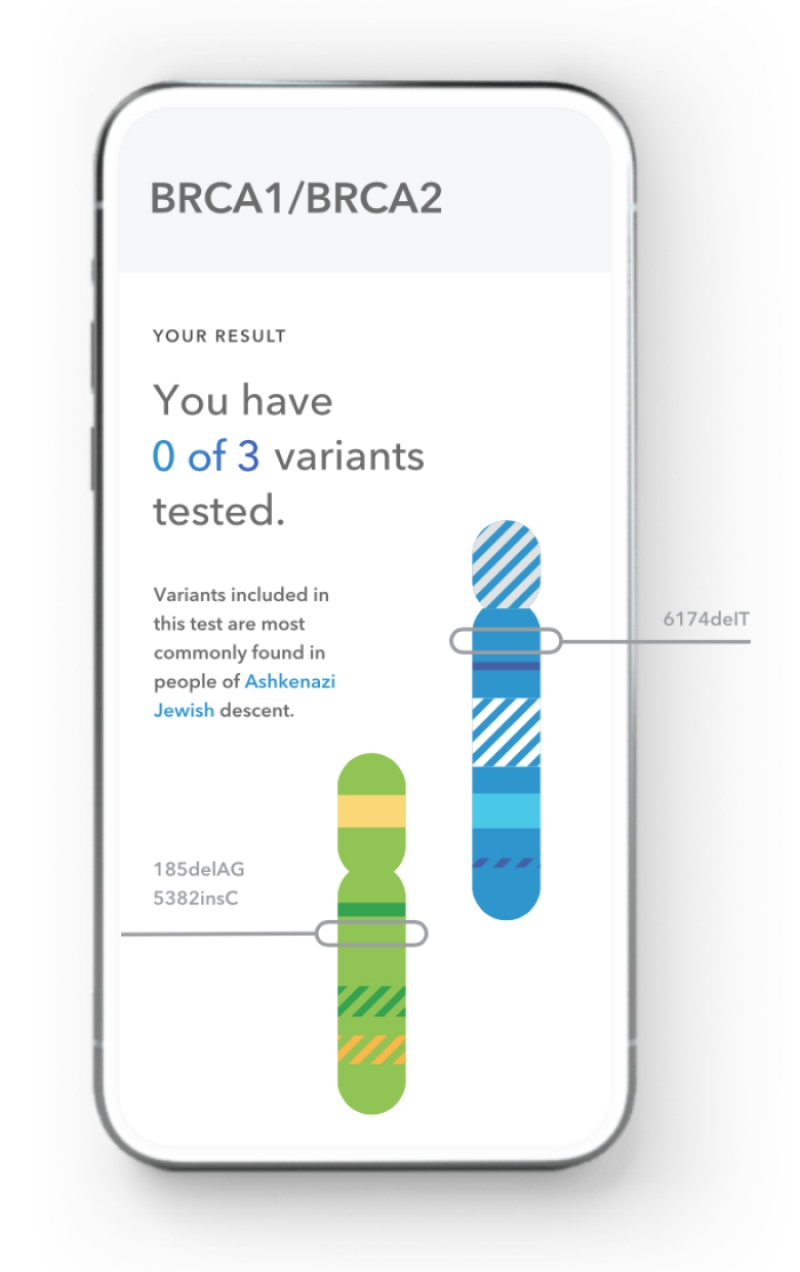
For example, more than 1,000 variants in the BRCA1 and BRCA2 genes are linked to a higher risk of breast and ovarian cancers. 23andMe tests for just three of them.
And knowing if you have a disease-causing BRCA variant matters. Women with some of those variants have a 45 to 70 percent lifetime risk of breast cancer and a 10 to 45 percent risk of ovarian cancer.1,2 (In fact, many experts advise those women to consider surgery to remove their ovaries and breasts as soon as they’re done having children.2)
With direct-to-consumer tests for BRCA variants, “people may experience unneeded anxiety or false reassurance,” cautions the National Cancer Institute.
“If you have a family history of breast cancer, do not rely on a direct-to-consumer genetic test to assess your risk,” says the CDC. Instead, see a geneticist or genetic counselor. Period. End of story.
2. Oversight is iffy
It’s the Food and Drug Administration’s job to keep tabs on direct-to-consumer test companies and to ensure that customers are getting clear, accurate information.
For most tests, though, the FDA does little or nothing.
“If the test claims to make a diagnosis, the FDA is supposed to regulate that,” says Alberto Gutierrez, former director of in vitro diagnostics at the FDA.
“But there are claims that fall into the category of wellness that the agency is not interested in seeing because they are considered low-risk,” he adds.
What’s wellness? Tests that predict, say, athletic ability, caffeine metabolism, or lactose intolerance.
“But it’s very much a gray area,” Gutierrez admits. “There are a lot of internal discussions at FDA about what is considered wellness.”
And the testing companies aren’t making things easier.
Everlywell, for example, claims that most of its tests are for “wellness monitoring, informational and educational use.” That includes its test for hemoglobin A1c, a long-term measure of blood sugar.
“It’s hard to see how that fits under wellness,” says Gutierrez, because doctors use hemoglobin A1c to diagnose diabetes.
The company does offer some tests—for Lyme disease and a handful of sexually transmitted infections—that it calls “diagnostic.” But other than a test for Covid-19, the FDA hasn’t authorized any of Everlywell’s diagnostic tests.
Why not? “The agency has been inconsistent about what they regulate,” says Gutierrez.
Sometimes, the feds seem to be on the job. For example, in 2013, the FDA ordered 23andMe to stop marketing genetic tests that told customers about their risk of disease. (The letter was signed by Gutierrez.)
In 2017, after the company submitted enough data to satisfy the agency, it got the FDA’s stamp of approval to tell users about their genetic risk for 10 diseases. And in 2018, 23andMe received the green light to test for three of the BRCA1 and BRCA2 mutations that occur more frequently in people of Eastern European Jewish descent.
“It’s difficult to know exactly why the agency hasn’t thrown the book at Everlywell, Lets Get Checked, and others,” says Gutierrez.
The FDA needs to step up, he adds.
“Consumers need a referee. Companies have a lot of incentive to make claims. And if somebody isn’t looking at the data behind those claims and making a judgment, you’re in a ‘buyer beware’ marketplace.”
3. Be skeptical of results for rare disease-causing variants
“Common genetic test often wrong when identifying rare disease-causing variants such as BRCA1 and BRCA2, study says,” ran the CNN.com headline in February.
“We had heard anecdotal reports from our clinical colleagues that patients were coming in with positive results from direct-to-consumer tests for rare disease-causing variants,” says Caroline Wright, a professor of genomic medicine at the University of Exeter in the UK.
That’s not just stressful; it could lead to unnecessary and invasive screening, treatment, or surgery.
The problem? A test called a SNP chip that wasn’t designed to detect rare genetic variants. (SNP—pronounced “snip”—stands for single-nucleotide polymorphism.)
“It’s the wrong tool for the job,” says Wright. The right tool? “Genome sequencing, which is very accurate for detecting rare variants.”
“We analyzed genetic data from nearly 50,000 adults who had both SNP chip and genome sequencing results,” Wright explains.
“The SNP chip was excellent for detecting common variants that are present in more than 1 in 100 people, as we expected. But as the variants got more rare—present in fewer than about 1 in 100,000 individuals—the SNP chip performed incredibly poorly. We were surprised at how bad it was.”
Of the roughly 4,800 rare variants identified by the SNP chip, 84 percent were false positives when tested against genome sequencing.3
And when Wright looked at rare variants in the BRCA1 and BRCA2 genes, nearly 95 percent of the positive SNP chip results were wrong.
Wright also looked at data on 21 adults who had both direct-to-consumer SNP chip tests and genome sequencing.
“We found that 20 out of 21 were falsely identified by the SNP chip as having at least one rare disease-causing variant,” she says.
“The message is that rare genetic variants detected by a SNP chip are far more likely to be wrong than right.”
4. Be wary of third-party services
The good news: “Many of the direct-to-consumer companies try their best to be responsible and only report rare variants that they have validated in-house,” says Wright.
The problem is that most companies also let you download your ‘raw’ data.
In a recent survey, 89 percent of people who had taken a direct-to-consumer genetic test downloaded their raw data. Of those, 94 percent reported using at least one third-party service—that is, another website—to interpret their results.4
Among them: SelfDecode.com, which allows you to upload your data from companies like 23andMe and Ancestry.
“Get comprehensive reports that analyze your genes and give suggestions to help you optimize specific health areas,” SelfDecode promises.
Of course, that assumes that the data you’ve uploaded to them is correct. If it’s not, “they could end up interpreting false results,” Wright warns.
5. It’s genetics. It’s complicated
“There are a lot of cases where genetic testing is essential,” says Wright.
For example, for rare diseases caused by a single-gene mutation, like Huntington’s disease, genetic testing can confirm a diagnosis that was based on symptoms.
And genetic testing can help people with a family history of a disease manage their risk and take preventive measures.
But that type of testing—which is best done under the guidance of a geneticist or genetic counselor—is meant to detect specific rare variants, not the hundreds of thousands of variants that direct-to-consumer tests analyze with a SNP chip.
Experts don’t even know what many of those variants mean for your risk of disease. Researchers have a term for them: “variants of uncertain significance.”
“I don’t think people appreciate how much variation there is in our genes,” says Wright. “The more you look, the more you find. But you don’t know what all that information means.”
“Getting a variant-of-uncertain-significance result is not uncommon, and it can be unsettling,” she notes. “As we sequence more people’s genomes, a lot of this uncertainty will resolve. Most of these variants are likely benign. For a few, we’ll realize that they cause disease.”
6. Genes are just a small piece of the puzzle
In most instances, “your genes are not determinative,” says Gutierrez.
“Common variants tend to explain much less of your risk than rare variants,” Wright explains. (Common variants are linked to diseases like diabetes and heart disease; rare variants are linked to diseases like cystic fibrosis.)
Instead, your lifestyle and environment have a greater impact on your risk than your genes.
Most of the information you get from a direct-to-consumer genetic test has limited value, says Gutierrez.
“Say a test tells you that you are at higher risk for diabetes. What are you going to do? You’re going to diet and exercise. Well, that’s what all of us should be doing.”
7. Hormone testing isn’t enough
Everlywell sells 32 direct-to-consumer tests, many of which measure hormones related to metabolism, fatigue, fertility, menopause, and more.
“The fundamental principle about hormone testing is that it only gives you a snapshot in time,” explains UCLA endocrinologist Rashmi Mullur.
“It tells you if the hormone is present and at what level. It doesn’t tell you if the hormone is working in your body.”
For example, Everlywell’s metabolism test measures thyroid-stimulating hormone, testosterone, and cortisol.
“By measuring your levels of each,” says the company’s website, “you can understand what you may be experiencing with your weight and energy.”
Don’t count on it.
“If a patient complains of having low energy or fatigue, I might test those hormones,” says Mullur. “But there are also non-hormonal tests of fatigue. I would also measure their electrolytes, I’d get a complete blood count, I’d test for iron deficiency, liver function, and so on.”
“In nine out of ten cases, I repeat my patients’ direct-to-consumer tests in my lab to confirm the results,” says Mullur.
“If I’m running other tests, I have to measure them again so that I can interpret the results as a unified bunch. It’s naive to think that you can get an answer about your health with a simple hormone test.”

8. Tests could lead to rash decisions
Scratching your head after looking at a direct-to-consumer test result?
Lets Get Checked allows users to discuss results with a nurse, while Everlywell offers a physician-led live webinar where you can ask questions. (If you test positive for, say, an STD, they offer a consult.)
But the nurses and physicians can only provide so much insight without knowing you or your medical history.
Mullur recommends talking with your doctor before making any big changes.
“When patients come in with direct-to-consumer test results, my first step is to figure out what they were trying to investigate,” says Mullur.
“Maybe they asked for the wrong test, maybe we need more testing, or maybe I can make a diagnosis based on their symptoms.”
And don’t forget the false positives from SNP chip tests for rare variants.
“If a test says that you have a rare gene variant and suggests a clinical action like screening or surgery,” says Wright, “work with a geneticist or genetic counselor to verify the finding.”
“Don’t put the cart before the horse.”
1 cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet.
2J. Natl. Compr. Canc. Netw. 19: 77, 2021.
3BMJ 2021. doi:10.1136/bmj.n214.
4Am. J. Hum. Genet. 105: 122, 2019.
Photo (top): Southworks/stock.adobe.com.
Continue reading this article with a NutritionAction subscription
Already a subscriber? Log in

